In this study, which was published in the journal Frontiers in Immunology on September 30th, researchers used sequencing to characterize the immune system of patients who survive from COVID-19 infection from symptom onset through recovery. Importantly, they also identified a potent biomarker for predicting disease progression. Follow-up studies could lead to the development of a treatment for COVID-19 that is inspired by our own immune system.
The study was led by Ling Chen and Nanshan Zhong of the National Clinical Research Center for Respiratory Disease in China and Jian Han, Faculty Investigator at the Hudson Alpha Institute in Alabama and founder of iRepertoire. Zhong is one of the doctors who first diagnosed SARS and was instrumental in treating and controlling the disease. Han was previously recognized for his work during the SARS outbreak, earning a Wall Street Journal Technology Innovation Award.
Now, Han, Zhong, and collaborators have taken insights from their experience with SARS and used them to take an unprecedented approach to studying COVID-19. For emerging viruses with no vaccine, our only defense is our immune system. This study provides an unprecedented level of insight into the immune cells of 23 COVID-19 patients over three different stages of the disease.
In order for our immune system to fight off a new infectious disease, it first has to learn to recognize it. That recognition is coordinated by a family of proteins called receptors that live on the surface of T cells and B cells.
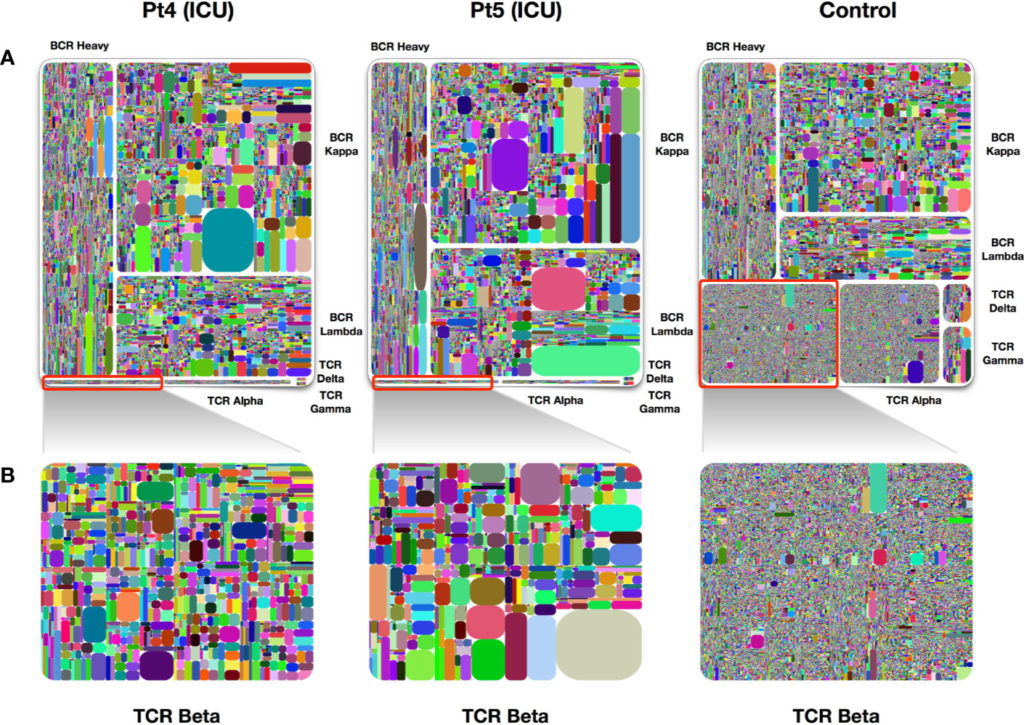
There are seven types of T cell and B cell receptor proteins, called chains, two of which combine to form the receptors on the surface of each B or T cell. Each individual chain is made up of multiple different segments, enabling millions of different unique B and T cells in every person.
When a new infection is introduced, the immune cells that recognize the invading virus multiply rapidly, causing a shift in the diversity of B and or T cells. By studying an infected person’s immune system fingerprint, known as the immune repertoire, we can gain insights into what kind of immune cells will be effective at fighting off the virus.
This study captured, for the first time, the expansion and contraction of all seven chains in the immune repertoire. They discovered that early in COVID-19 infection, T cell discovery is significantly depleted. T cells recovered as patients improved, suggesting that the T cell repertoire might be an important marker for predicting disease progression.
For B cells, the chain composition of receptors can indicate whether the B cell has become “activated” by an infection. Activated B cells switch their chain type (from D/M to A/M, or G/M) and begin producing antibodies. Determining which specific chains are activated might help identify what antibodies will be effective in treating the infection. Chen and colleagues discovered that patients infected with COVID-19 exhibit a prominent expansion of their M- and G-type chains, followed by a later transition to A-type chains.
“The next step is to isolate individual B cells that are exhibiting chain switching in order to identify the antibodies produced by patients who recover from infection,” said Han. “We are continuing this work at iRepertoire by performing network analysis on the B cell data from these patients and identifying responding clones. We are also participating in a local study to use our single cell sequencing technology on samples from infected patients by directly identifying Sars-Cov-2-specific B cells. Both methods can reveal the identity of neutralizing antibodies of therapeutic value.”
“What really makes this study interesting, is that we profiled all seven chains of the immune repertoire at the same time,” said Miranda Byrne-Steele, Director of Research and Development at iRepertoire and an author on the paper. “Most studies look at one or two chains at a time. By profiling all seven chains, we identified patterns that you wouldn’t have noticed in a single chain study.”
Those patterns have potential clinical significance. For T cells, the signature observed in patients that recover versus those that progress, could aid in the development of prognostic tests. Such tests might help identify which patients are likely to need or benefit from particular treatments. For B cells, those that proliferate might point to antibodies that can themselves serve as potential treatments for people who are already infected, but not recovering.

About iRepertoire
Founded in 2009 at the Hudson Alpha Institute for Biotechnology in Huntsville, AL, iRepertoire was the first company to develop and commercialize immune repertoire sequencing technology and products. Over the past decade, iRepertoire has continuously improved our legacy technology, arm-PCR, which allows researchers to inclusively amplify all of the expressed V(D)Js in either B or T cells, and introduced dam-PCR, the only technology on the market with the ability to profile all 7-adaptive immune chains in the same assay with the inclusion of unique molecular identifiers. Continuing tradition as leaders in the industry, our single cell service, iPair, is the first consumer-based service, specifically designed for capturing physically paired variable regions in T cells and B cells.